President Donald Trump has promised to officially declare the opioid epidemic a “national emergency.”
“We’re going to have a major announcement, probably next week, on the drug crisis and on the opioid massive problem, and I want to get that absolutely right,” Trump said in a press conference last Monday with Senate majority leader, Mitch McConnell. “This country and, frankly, the world has a drug problem. But we have it and we’re going to do something about it.”

However, opioid abuse amongst military veterans rarely receives headlines, despite vets being more prone to addiction compared to the American civilians they protect.
“The opioid epidemic has impacted veterans, and overdose deaths among veterans remain elevated when compared to the civilian population,” said Dr. John D. Daigh, Assistant Inspector General for Healthcare Inspections.
Military veterans are at a higher risk for opioid abuse because they are prescribed painkillers at a much higher rate than ordinary Americans. Just under 5 million opioid prescriptions were dispensed to 877,253 veterans in FY 2016. That’s 43% more prescriptions than the average rate for civilian Americans, according to The Center for Investigative Research. It should also be noted that this data is only obtained from VA outpatient pharmacies, and does not include opioid prescriptions written by non-VA pharmacies or prescriptions paid for directly by the veteran.

“While about 30 percent of the nation’s adult population experiences chronic pain,” says Dr. Carolyn Clancy, VA’s chief medical officer, “the problem of chronic pain in VA is even more daunting, with almost 60% of returning veterans from the Middle East and more than 50% of older veterans in the VA health care system living with some form of chronic pain.”

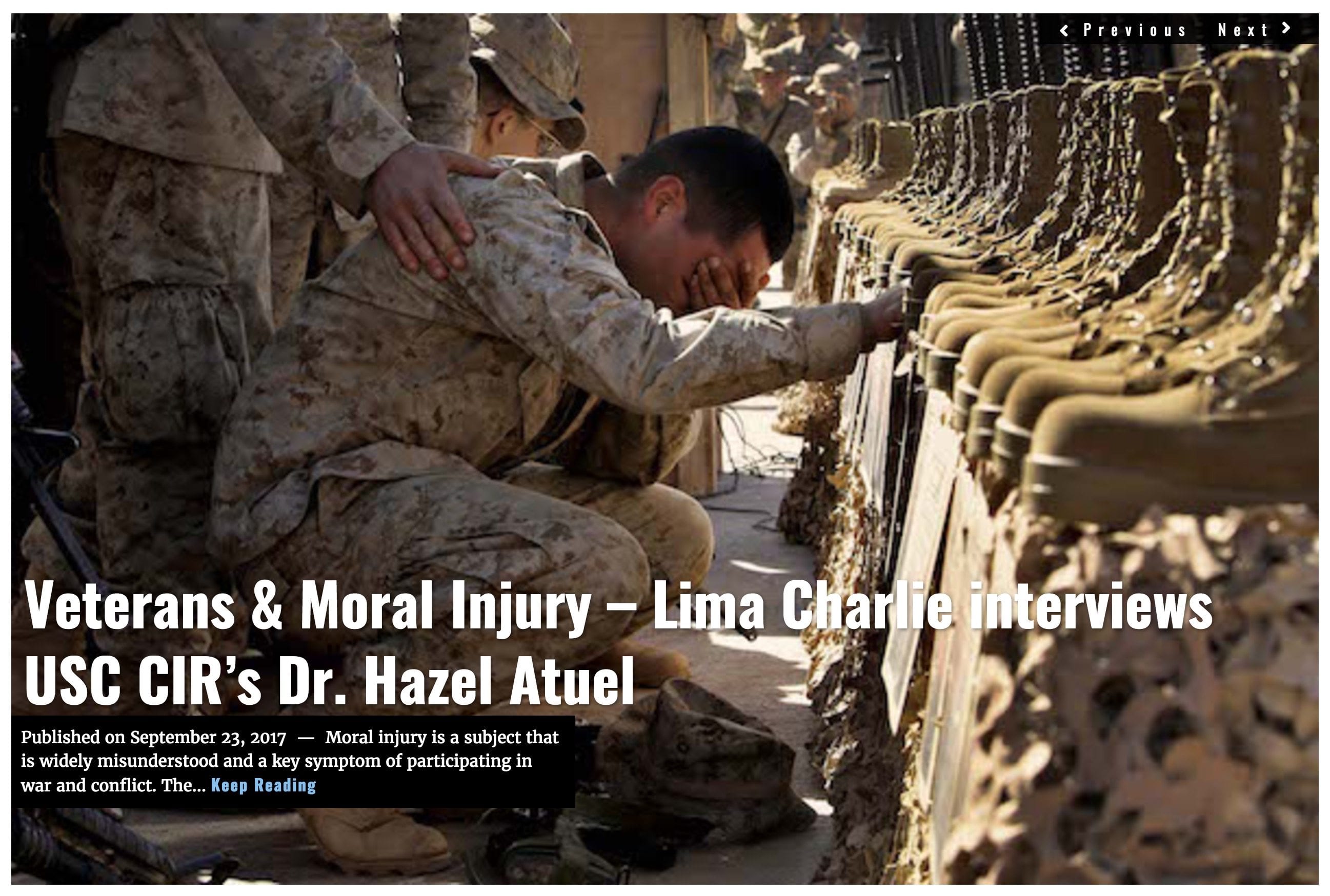
Whenever someone is prescribed opioids – regardless of veteran/civilian status – they are are prone to developing an addiction. But if a veteran is diagnosed with PTSD and simultaneously experiencing chronic pain, that pain may trigger traumatic memories and hyper-aroused states, which only exacerbate the pain. This vicious cycle, which researchers call the “Mutual Maintenance” hypothesis, further increases the risk in veterans for opioid abuse and dependence.
What does declaring a National Emergency entail?
The reasons for declaring the opioid epidemic a national emergency seem clear based on the evidence. But the process for declaring a national emergency is much less obvious.
When President Trump announced his plan to declare the opioid epidemic a national emergency last Monday, the rest of his White House staff began scrambling to develop a policy. The official emergency declaration is expected to come later this week when that policy is ready, so we will soon know what the White House’s response will entail.
As far as executive action goes, however, there are two ways the president can approach the crisis through an emergency declaration.
Option #1 is the Stafford Act
Commonly used by state governors following a natural disaster, this option would let President Trump declare a national emergency and force a response to the opioid crisis through the Federal Emergency Management Agency (FEMA). This option seems unlikely, however, considering the onslaught of hurricanes in Texas, Florida, and Puerto Rico this year. FEMA’s resources – both physical and financial – are dwindling after those three disasters.

Option #2 is the Public Health Service Act
Rather than calling on FEMA, the president can call on Health and Human Services Secretary, Eric Hargan, to declare a Public Health Emergency on opioids. This would give the White House access to a “preparedness and response” fund, known as ASPR, which is appropriated $1.5 billion each year by Congress, on average.
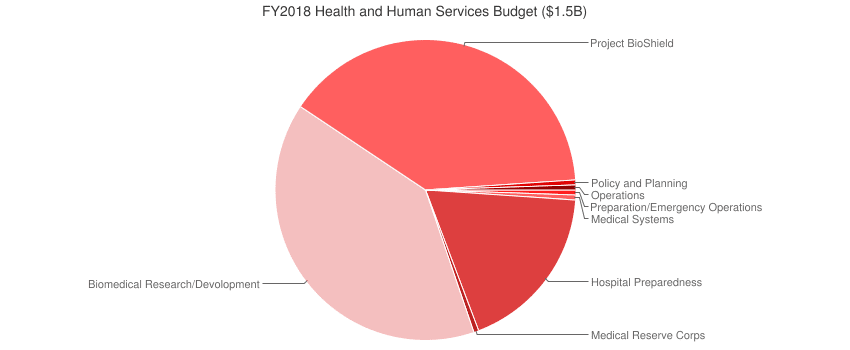
However, much of that public health funding is budgeted towards the flu, emerging infectious diseases (such as Ebola and Zika), and other “chemical, biological, radiological, and nuclear threats,” so it is unclear how much funding remains available. One HHS spokesperson claims there is only $57,000 left, according to Politico.
Regardless of how the emergency response is rolled out, Jay Butler, Alaska’s chief medical officer, from a state where opioid prescriptions are some of the highest in the nation, wants to remind Americans that change will come slowly.
“There are no silver bullets,” Butler told Politico. “We can’t get distracted on unicorn hunts thinking there’s one solution to solving the complex issue of the opioid crisis. It’s not a problem that will be quickly or easily resolved.”
If you are a veteran struggling with addiction and want to share your story, please contact our team of reporters here.
James Fox and Heather L. Rusch, Lima Charlie News
Heather L. Rusch is a Clinical Investigator at the National Institutes of Health (NIH) and Henry M. Jackson Foundation for the Advancement of Military Medicine, Center for Neuroscience and Regenerative Medicine, Bethesda, MD.
Lima Charlie provides global news, insight & analysis by military veterans and service members Worldwide.
For up-to-date news, please follow us on twitter at @LimaCharlieNews
In case you missed it:


![Image Memorial Day may soon be a remembrance of democracy and those who had the courage to defend it [Lima Charlie News]](https://limacharlienews.com/wp-content/uploads/2018/05/Memorial-Day-may-soon-be-a-remembrance-of-democracy-and-those-who-had-the-courage-to-defend-it-Lima-Charlie-News-480x384.png)
![A Trump war crime pardon dishonors us all [Lima Charlie News]](https://limacharlienews.com/wp-content/uploads/2019/05/A-Trump-war-crime-pardon-dishonors-us-all-Lima-Charlie-News-480x384.png)
](https://limacharlienews.com/wp-content/uploads/2019/03/Remembering-Becket-A-mothers-search-for-answers-480x384.png)



![The Mind of Bolton - AUMF and the New Iran War [Lima Charlie News]](https://limacharlienews.com/wp-content/uploads/2019/05/Inside-the-mind-of-Bolton-Lima-Charlie-News-main-01-480x384.png)
![Image Memorial Day may soon be a remembrance of democracy and those who had the courage to defend it [Lima Charlie News]](https://limacharlienews.com/wp-content/uploads/2018/05/Memorial-Day-may-soon-be-a-remembrance-of-democracy-and-those-who-had-the-courage-to-defend-it-Lima-Charlie-News-150x100.png)
![A Trump war crime pardon dishonors us all [Lima Charlie News]](https://limacharlienews.com/wp-content/uploads/2019/05/A-Trump-war-crime-pardon-dishonors-us-all-Lima-Charlie-News-150x100.png)